Depression & Mental Health in America
Posted: October 28th, 2022
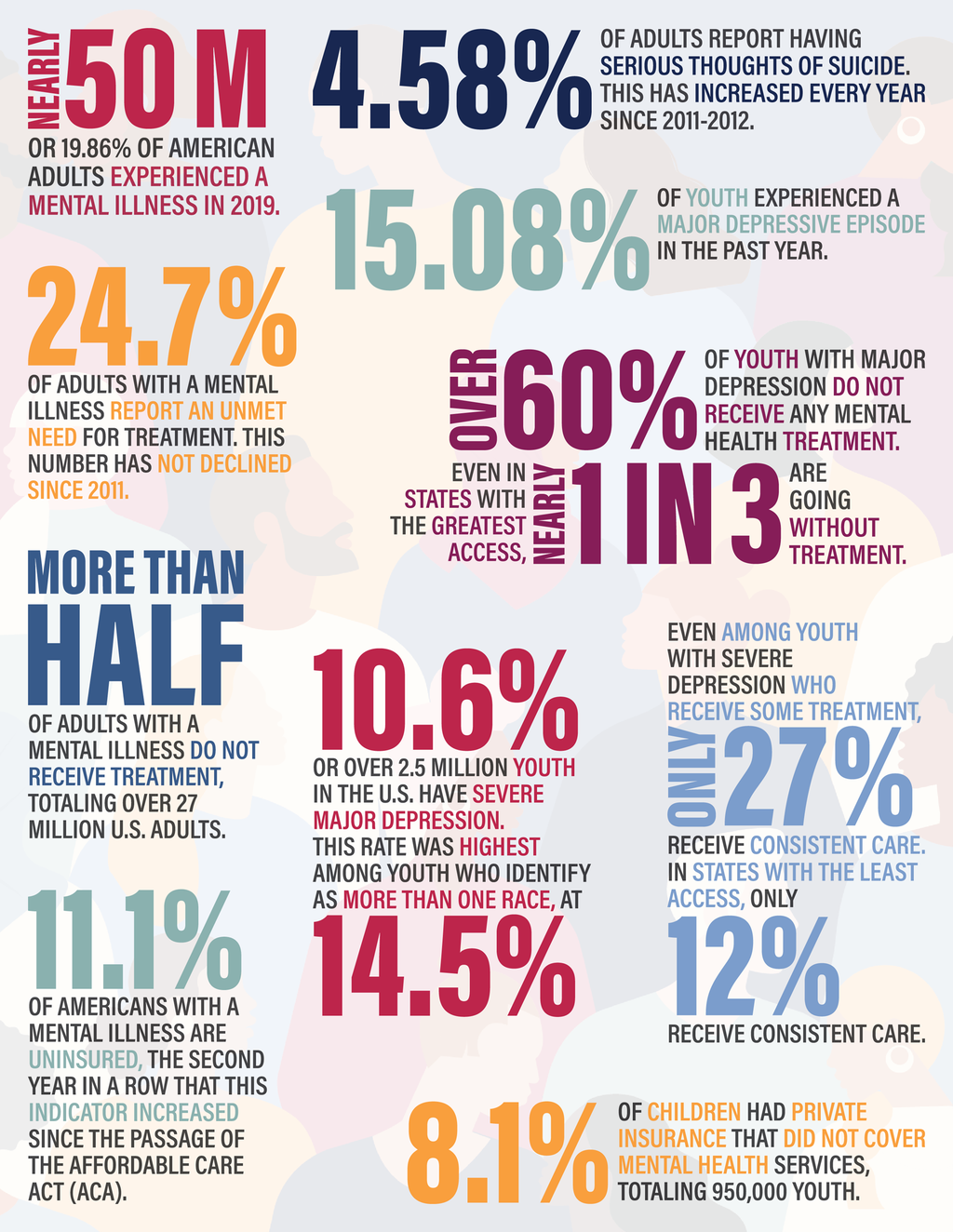
- In 2019, just prior to the COVID-19 pandemic, 19.86% of adults experienced a mental illness, equivalent to nearly 50 million Americans.
- Suicidal ideation continues to increase among adults in the U.S. 4.58% of adults report having serious thoughts of suicide, an increase of 664,000 people from last year’s dataset. The national rate of suicidal ideation among adults has increased every year since 2020-2021. This was a larger increase than seen in last year’s report and is a concerning trend to see going into the COVID-19 pandemic.
- A growing percentage of youth in the U.S. live with major depression. 15.08% of youth experienced a major depressive episode in the past year, a 1.24% increase from last year’s dataset. In the bottom-ranked states, up to 19% of youth ages 12-17 experienced major depression.
- Over 2.5 million youth in the U.S. have severe depression, and multiracial youth are at greatest risk. 10.6% of youth in the U.S. have severe major depression (depression that severely affects functioning). The rate of severe depression was highest among youth who identified as more than one race, at 14.5% (more than one in every seven multiracial youth).
- Over half of adults with a mental illness do not receive treatment, totaling over 27 million adults in the U.S. who are going untreated. In Hawaii, the bottom-ranked state, 67% of adults with a mental illness did not receive treatment. Even in Vermont, the top-ranked state in the U.S., 43% of adults experiencing a mental illness were not receiving treatment.
- The percentage of adults with a mental illness who report an unmet need for treatment has increased every year since 2011. In 2019, 24.7% of adults with a mental illness report an unmet need for treatment.
- Over 60% of youth with major depression do not receive any mental health treatment. Even in states with the greatest access, nearly one in three are going without treatment. In Texas, the bottom-ranked state for this indicator, nearly three-quarters of youth with depression did not receive mental health treatment.
- Nationally, fewer than 1 in 3 youth with severe depression receive consistent mental health care. Even among youth with severe depression who receive some treatment, only 27% received consistent care. In Tennessee, the bottom-ranked state, that rate is as low as 12%. 65.6% of youth in Maine (ranked 1st) received consistent treatment, which is 16% higher than Vermont (49.7%) which is ranked 2nd.
- Both adults and youth in the U.S. continue to lack adequate insurance coverage. 11.1% of Americans with a mental illness are uninsured. There was a 0.3% increase from last year’s dataset, the second year in a row that this indicator increased since the passage of the Affordable Care Act (ACA). 8.1% of children had private insurance that did not cover mental health services, totaling 950,000 youth.
- Rates of substance use are increasing for youth and adults, even prior to the COVID-19 pandemic. 7.74% of U.S. adults and 4.08% of youth had a substance use disorder in the past year. Substance use increased 0.07% for adults and 0.25% for youth over last year’s report.
This year’s report includes spotlights on two of MHA’s policy priorities in 2021-2022 – the implementation of 988 as the national three-digit suicide prevention and mental health crisis hotline and increasing mental health education and supports in schools, particularly for BIPOC youth.
- Suicidal Ideation and 988 Implementation: With the passage of the new 988 number for suicide prevention and mental health crises, there is an opportunity to create a continuum of crisis care with adequate funding that ensures mental health responses to mental health crises and prioritizes equity, particularly for BIPOC individuals. However, Of the 13 states (ranked 39-51) with the highest rates of suicidal ideation among adults, only four have successfully passed state legislation for 988 implementations: Utah, Oregon, Indiana, and Colorado. Of these, only one currently includes user fees.
- Disparities in Mental Health Treatment for Youth of Color: White youth with depression were most likely to receive mental health treatment, and Asian youth were least likely to receive mental health care. Youth of color with depression, particularly Native American or American Indian, multiracial, and Black youth, were most likely to receive non-specialty mental health services in education settings. To create healthier communities, and to better serve students of color who may only receive mental health services in educational settings, schools need long-term financial support to build up sustained and sufficient school infrastructure.
Explore the Web Based Report Here
The State of Mental Health in America
In the above links you will find a Collection of Data across all 50 states and the District of Columbia answering the following questions:
- How many adults and youth have mental health issues?
- How many adults and youth have substance use issues?
- How many adults and youth have access to insurance?
- How many adults and youth have access to adequate insurance?
- How many adults and youth have access to mental health care?
- Which states have higher barriers to accessing mental health care?
Our Goal:
- To provide a snapshot of mental health status among youth and adults for policy and program planning, analysis, and evaluation.
- To track changes in the prevalence of mental health issues and access to mental health care.
- To understand how changes in national data reflect the impact of legislation and policies.
- To increase dialogue and improve outcomes for individuals and families with mental health needs.
Why Gather This Information?
- Using national survey data allows us to measure a community’s mental health needs, access to care, and outcomes regardless of the differences between the states and their varied mental health policies.
- Rankings explore which states are more effective at addressing issues related to mental health and substance use.
- Analysis may reveal similarities and differences among states in order to begin assessing how federal and state mental health policies result in more or less access to care.